High above Sutter Street in downtown San Francisco, a team of Global Viral Forecasting Initiative (GVFI) scientists is hard at work studying how the next viral epidemic might be contained or prevented.
From its sixth-floor office, the group has a clear view of the bustling city around them, a fitting reminder of the enormous scale of the work. Tribal artwork hangs from the walls in the office, directly across from a world map dotted with the organization’s different field sites around the globe.
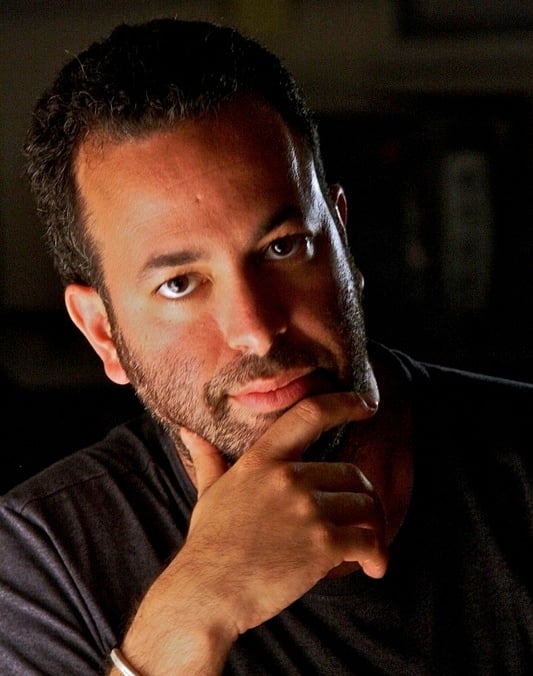
It is here that GVFI founder and CEO, Nathan Wolfe ’92, coordinates the organization’s multipronged approach to combatting epidemics. Wolfe, the Lorry I. Lokey visiting professor in human biology at Stanford, has received a great deal of coverage in the media for his work in recent years. In 2011, he was named one of Time Magazine’s 100 most influential people in an article that called GVFI “the CIA of infectious disease.” Wolfe published a book that same year, “The Viral Storm,” detailing his work in the context of the historical interaction between humans and viruses.
Wolfe left his tenured professorship at UCLA in 2008 to found GVFI and change the way scientists fight epidemics. In an increasingly globalized and interconnected world, the possibilities for an epidemic to take hold are greater than ever before, but so are the resources available to stop one. The problem Wolfe and others witness, however, is that the current strategies are often more focused on responding to pandemics than working to avoid them in the first place.

“Not too long ago, people said that the best way to stop a heart attack was to actually wait for the heart attack to occur, then do bypass surgery,” Wolfe said. “About 10 years ago, it became clear to a small number of us [scientists] that what had happened in individual medicine, where it had become very obvious that an ounce of prevention was worth a pound of cure, also made sense on a population level.”
As a boy, Wolfe was drawn into the world of science by a particular fascination with some of humanity’s close relatives, the chimpanzees and the gorillas. He remembers watching a National Geographic documentary that detailed the close genetic connection between humans and apes. This portrayal clashed with his memories of going to the zoo, where a clearly defined hierarchy separated humans and animals, often by iron bars.
“I remember the idea that by interrogating nature and studying it, you could fundamentally change the way we saw the world,” Wolfe said, reflecting on the memory.
Wolfe’s fascination with apes continued into his adult life, leading him to conduct field research in Africa as a graduate student at Harvard. The experience paved the way for many years of work in the field and his future path in virology.
During his time in the field, Wolfe would contract malaria three different times, the last of which nearly killed him. It is not hard to see why he is sometimes known as “the Indiana Jones of virus hunters” among professionals in his discipline.
Through sometimes perilous field research, Wolfe gleaned valuable insights into some of the avenues of transmission that viruses can take. In particular, Wolfe recognized the tremendous danger of viruses jumping from animals to humans when local hunters prepared meat. Many of the viruses that affect humans originate in animals, and the interspecies leap is rarely easier than during the close and intimate contact of butchering.
Though monitoring such activity in rural parts of Africa is often difficult and costly, technological innovations are allowing scientists like Wolfe to track viruses in a way they simply could not before.
“Fifteen or 20 years ago, the best we could do was to be able to look at viruses that were cultured in the laboratory,” Wolfe said. “Now new sequencing technologies allow us to look at the sum total of genetic diversity in a particular specimen, so we’re finding viruses that we otherwise would not [have].”
Members of Wolfe’s team at GVFI put these technologies to use when investigating a recent virus outbreak. They discovered a previously unrecorded virus using deep sequencing techniques. Methods available even a year or two ago would have completely missed the virus, due to its low concentration in the samples studied. The group plans to publish these findings in the coming months.
A critical part of fighting epidemics is simply identifying a given virus, which can offer insights into how quickly the virus will spread, how deadly it might be and what response is appropriate in order to contain it. For example, the human immunodeficiency virus (HIV), the virus responsible for acquired immunodeficiency syndrome (AIDS), went unidentified and untreated for decades in human populations. Wolfe called this “a stunning failure in human health services.” In order to prevent this from happening again, GVFI has innovatively used local hunters in Africa to collect dried blood samples of their kills, which are later sent to labs for analysis.
In the years since Wolfe began working on preventing epidemics, a growing recognition has emerged in governments and organizations around the world about the need to adopt a more proactive approach to combatting viruses, especially in places where viruses are easily transmitted from animals to humans.
“It’s exciting for me because now there are a number of young organizations that are starting to do this work, and it’s becoming more of an ecosystem where folks are approaching different angles about how to address these problems,” Wolfe said.
Wolfe also noted the importance of more traditional structures like the World Health Organization (WHO) and the Center for Disease Control (CDC), both of which GVFI regularly coordinates with as part of the WHO Global Outbreak Alert and Response Network. But Wolfe believes the old model is rapidly disappearing.
“Scientists in those [traditional] institutions recognize that they have a lot of limitations in terms of their mission, in terms of their funding and in terms of their ability to move quickly,” Wolfe said. “I think it’s clear to all of us now that the world in five or 10 years is going to look a lot different than it does now in terms of the kinds of structures out there.”
Though GVFI now has staff working in six different African and Asian countries, Wolfe plays more than just the role of administrator as CEO. He still regularly goes out into the field to conduct research and is closely involved in the collaborative analysis of the viruses. Wolfe also brainstorms directly with many of GVFI’s local scientists in Africa, Asia and elsewhere around the world about the best approaches to engaging with the local populations.
Under Wolfe’s guidance, GVFI has expanded into a number of diverse areas for tracking viruses. Wolfe’s background makes him well suited for this kind of innovation, as he sees a parallel between his undergraduate education in human biology (HumBio) at Stanford and the company’s interdisciplinary and collaborative approach to problem solving.
“We work with computer scientists, a lot of virologists, a number of epidemiologists, and one of my team members is a medical anthropologist,” Wolfe said. “The way my career has worked out is fundamentally ‘HumBio’ in a sense. It’s just, pick a problem and pick whatever sorts of disciplines are necessary to effectively address the problem.”
Over the past couple of years, GVFI has also pursued the burgeoning field of digital epidemiology. Tapping into the massive amounts of data available through the Internet, digital epidemiology allows scientists to forecast trends in illness without ever leaving the laboratory. For example, epidemiologists are exploiting the online availability of over-the-counter drug sales records to make short-term predictions about sickness, according to The Atlantic.
On Wolfe’s team, Stephanie Nevins ’11, a GVFI intern and Wolfe’s former student, is currently exploring data mining techniques for extracting information from social networks to plot trends in epidemics.
During her senior spring at Stanford, Nevins took Wolfe’s Viral Lifestyles seminar. For the class, she worked on a project that eventually turned into a formal business plan to overhaul the way patients interface with their medical provider, which attracted Wolfe’s attention.
“In his class, we really asked big questions about how we can change the way we think about public health,” Nevins recalled. “It was so interesting to realize that you could study disease in populations in high-risk places and actually have the ability to stop them before they spread.”
Wolfe is also able to balance this broader view with a sense of pragmatism in his teaching.
“He is one of the most approachable, thought-provoking professors I have interacted with at Stanford,” said Kasey Kissick ’12, who also took the seminar. “He teaches in a very practical manner, leaving students with a sense of guidance and direction, rather than just a collection of abstract concepts and facts.”
Toward the end of “The Viral Storm,” Wolfe writes about the necessity of establishing a 24-hour “situation room” as a command and control center for preventing epidemics. The organization would employ the innovative management of a Silicon Valley start-up to do a variety of tasks, such as sorting massive amounts of data, maintaining regular contact with global health leaders and using a series of field sites to monitor the situation on the ground.
While Wolfe writes that no such situation room exists today, the office above Sutter Street doesn’t appear far from his vision.