Sex is great. Safe sex is even greater. With so many options for protection available, having safe sex has never been easier. However, it can often seem as though the status quo is using just condoms or the pill — an impression that is somewhat limiting. What about encounters other than cis-hetero vaginal intercourse, where pregnancy isn’t a concern but the prevention of sexually transmitted infections (aka STIs or STDs) is? What’s available on campus, what are people’s perceptions of various methods of protection and birth control, and is there enough being done to combat the cisnormativity and heteronormativity that tends to be woven into sex education and conversations about birth control?
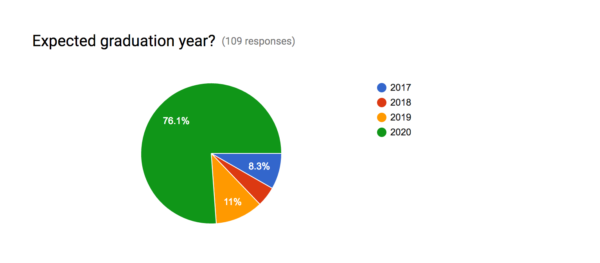
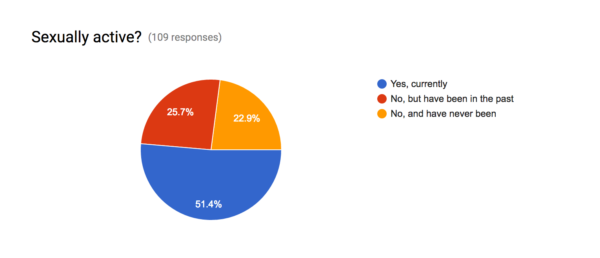
A small, informal survey to which 109 Stanford undergraduates responded addresses some of these questions, although it is abundantly clear that many more questions remain to be asked and answered and that a larger and more formal survey ought to be conducted to dig even deeper into this topic. Of the respondents to the survey, roughly 75 percent were freshmen and a little over half of the respondents described themselves as being currently sexually active.
When asked what their preferred methods of protection against STIs or general methods of birth control are, or would be in the case that they do not currently use protection/birth control, respondents listed external condoms and oral contraceptives among their top choices. However, several other methods, such as intrauterine devices (IUDs) and abstinence, also received wide support. It should be noted that this question was directed towards protection against STIs as well as the prevention of pregnancy. However, the prevention of pregnancy would not be a concern in cases of sex that isn’t cis-hetero penetrative sex, and the survey (drafted by yours truly) ought to have included more detailed language and further options to clarify this.
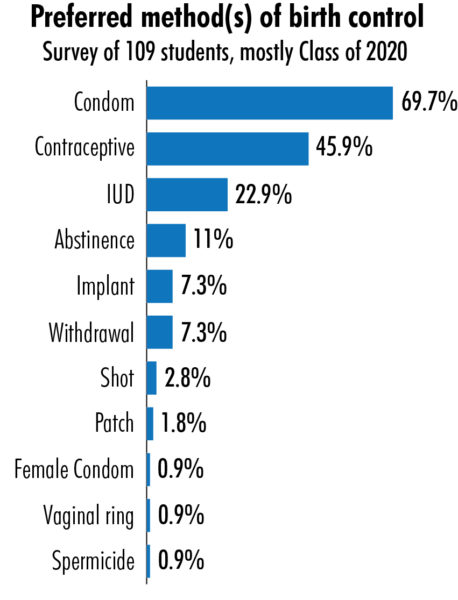
(Response options for this question: external condoms, oral contraceptives, birth control implant, birth control patch, withdrawal “pullout” method, birth control shot, IUD, birth control sponge, abstinence, vaginal ring, cervical cap, diaphragm, female condom, fertility awareness-based methods, spermicide, vasectomy, sterilization for women, dental dam.)
The motivation behind conducting this survey was to determine not only what kind of protection Stanford students employ but also where Stanford students get their birth control from and what general perceptions of different kinds of birth control may be. The majority of respondents wrote that they either purchase protection at pharmacies, such as CVS, or receive birth control through their personal doctors. Others wrote that they make use of services such as Planned Parenthood. A minority stated that they make use of the Stanford Sexual Health Peer Resource Center (SHPRC) and/or their PHEs.
The process of finding the kind of protection/birth control best suited to you is often ongoing. When asked whether they were considering changing their current methods of birth control/protection, many respondents who answered “yes” often cited desires for greater convenience, efficacy and permanence in their reasoning. Regarding reliability of forms of birth control, there was some variance in perceptions of the most reliable methods, which is to be expected given the wealth of options available. IUDs, abstinence and various combinations of condoms and hormonal methods were frequently mentioned. However, a vast majority of respondents seemed to agree that chief among the least reliable forms of birth control would be withdrawal (“the pullout method”).
Although this survey barely begins to skim the surface of the use and perceptions of birth control on Stanford’s campus, it did provide some valuable insights. When asked whether they had any recommendations or complaints regarding how Stanford distributes birth control/protection and educates students about safe sex, many respondents had illuminating feedback to offer. Several final takeaways were as follows:
- SHPRC is an excellent resource that should receive greater attention.
- Mandatory education about safe sex practices would be beneficial, as students may not have had access to adequate sex education prior to coming to Stanford.
- Condoms should be more widely distributed on campus, and options beyond condoms should be more readily available.
- Heteronormativity and cisnormativity remain problematic factors in discussions about sex and birth control.
So, armed with these new tidbits of knowledge, I urge you to go and seek out as much information as you can. Then, having fortified yourself with a broad understanding of the myriad of options out there, continue doing whatever (or whomever) works best for you.
Contact Cecilia Atkins at catkins ‘at’ stanford.edu.