As of mid-July, Stanford’s reopening plan will continue forward as California sees a surge of coronavirus cases, with confirmed cases having more than doubled in the last month. Stanford researchers weigh in on important considerations for preventing the spread of COVID-19 on campus.
This new surge in coronavirus cases is affecting a younger demographic, with over 60% of new infections identified among people ages 18 to 49. Eran Bandavid M.S. ’09, an associate professor at Stanford Medicine, said that this is likely due to the relaxing of stay-at-home efforts.
“It’s younger people getting infected more, because it’s younger people who are going out,” Bandavid said. He added that people in this age range are also, generally speaking, at a lower risk for health complications from COVID-19, allowing them to spread the disease to others asymptomatically without evening knowing it.
“If they get infected, then they recover,” he said. “If you look at California, the entire state has zero people under the age of 17 who’ve died of Covid-19 through July 7. So, you know, is it dangerous? I mean — it depends what you mean by dangerous.”
Bendavid added that while a rise in the number of cases is expected with reopening, the dialogue around COVID-19 tends to be overly-fixated on infection rates, while all other considerations, such as sacrifices to student education and economic repercussions, take the backseat.
“The unidimensional discussion of the coronavirus allows us to ignore these other costs, and I wish that there is a more balanced consideration of what it means for Stanford to have more infections,” he added. “What number of infections would be acceptable in order to allow students to have their college experience?”
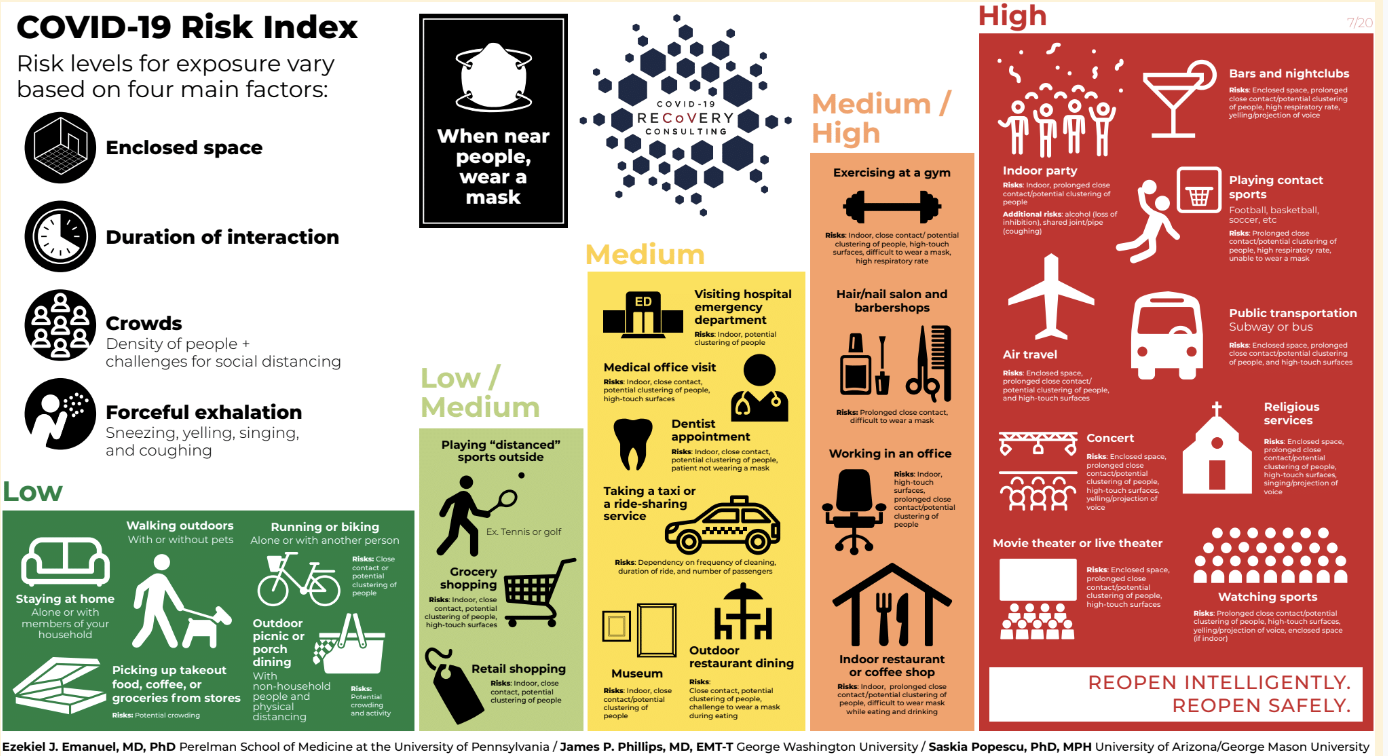
Conclusive research has shown that the coronavirus can remain suspended in the air in aerosol particles, contributing to the wide public emphasis on precautions such as wearing masks, hand washing and social distancing protocols. However, recent studies have shown that significant traces of the virus remain on the ground, as airborne droplets fall to the floor after someone coughs.
“These aren’t things that people naturally expect,” said Anesthesia Informatics and Media Lab senior research scientist Amy Price. “They found that there [traces of the virus] on the floor and people were tracking it in and out with their shoes. The media and everything we see is saying [to use] masks and hand washing,” but that “carries our mind away from the fact that yes, it could very easily drop to the ground.”
Various metrics have been identified as benchmarks for reopening by the CDC. On the frontlines, this means the ability to “screen large numbers of symptomatic patients safely” and achieving “more discharges than admissions for COVID-19” in hospitals in the area.
“The [reopening] plan assumes that you have the ability to test people to make sure that they’re coming in and they’re not sick, and that they’re not going to infect other people,” said Yvonne Maldonado, a pediatric infectious diseases professor. “You have to have a way to contact trace people, to trace individuals who are exposed to that person, [then] you have to isolate people and take care of people if they get sick.”
The question of reopening also highlights the potential power of design thinking for adapting to a post-pandemic world.
“Design thinking could be involved where we ask end users, including students, older people, and professors, and everyone how they would make physical distancing better,” Price said “How could they make masks that communicate? How could they make something about COVID fun? How would they choose to take away the fear [surrounding COVID]?”
The scientific community believes that, once reopening begins, there is a risk of having to close public spaces and return to lockdown. Price says this will require defining metrics to decide when lockdown should resume. For example, if there is a sharp increase in the number of infected health care workers or more COVID admissions than discharges in the hospital.
Some of the biggest questions will be how much community transmission is there going to be, and how can we control that on campus? For Maldonado, the best way to do that is to have everybody who comes onto the campus follow all the basic rules, which [includes] social distancing, masking, hygiene and following the guidance [of the medical community].”
Contact Rachel Kavalakatt at rkavalakatt ‘at’ gmail.com.