After passing over front-line residents and fellows for the first wave of COVID-19 vaccinations, Stanford Medicine has created a new allocation method that places more weight on COVID-19 exposure in clinical settings, according to a statement from Stanford Medicine leadership obtained by The Daily.
On the morning of Dec. 18, over 200 residents and fellows protested Stanford Medicine’s vaccine rollout plan, which allocated only seven of 5,000 available doses to front-line housestaff, according to an open letter written by the Chief Resident Council. Stanford Medicine has since apologized for the mistake and worked to revise their original distribution plan.
As of Monday night, more than 600 residents and fellows and nearly 4,000 total patient-facing healthcare workers had been vaccinated, according to Stanford Health Care Chief Medical Officer Niraj Sehgal. Individual departments, rather than the original algorithm, are now determining who is eligible to receive the vaccine first.
The first wave, which will end on Dec. 28 and aims to vaccinate 8,000 healthcare workers, is inclusive of all patient-facing health care workers, including ICU nurses, respiratory therapists, food services staff and environmental services staff. The first tier of vaccines will be distributed by the end of the month, the second tier by early January and the third tier by the end of January.
“The algorithm sounded nice and it was very fancy, but obviously had a lot of pitfalls,” said neurocritical care fellow Spencer Craven. “They’ve abandoned that for a more straightforward approach, in which they simply emailed the department heads and said ‘Can you please provide us a list of people who are at the highest risk?’”
Additional shipments of the vaccine are expected to arrive in the next few days, and Stanford Medicine is currently on track to provide vaccine doses to all front-line healthcare workers by the end of this month, according to surgery department chair Mary Hawn. According to a statement to the pediatrics department from department chair Mary Leonard, Stanford expects to receive nearly 25,000 doses by the end of the year.
The original allocation method was based on an algorithm intended to determine prioritization order. According to a slide from Stanford Health Care, it took into account variables such as age, prevalence for COVID-19 and California Department of Public Health guidelines, assigning employees a score between 0 to 3.48 based on these factors. The higher the score that employees received, the higher they would be prioritized.
According to Leonard, the algorithm intended to prioritize higher-risk healthcare workers older than 65 and younger than 25. It also prioritized those from highly impacted communities and people “at greatest risk of transmission from outside the hospital”–– factors that insufficiently took into account the risk of exposure while at work. This allowed attendings working from home and senior faculty to qualify before younger residents and fellows who rotate between units and directly treat COVID-19 patients.
The model included variables that were similar to other hospitals around the country, Sehgal wrote in a statement to The Daily. However, depending on how these variables are weighted, models from different hospitals will prioritize healthcare workers differently.
“If one weighted those who are likely to have severe illness/death, or communities most impacted by COVID-19 working in hospital settings, younger health care workers could be less prioritized,” he wrote. “If one weighted those directly caring for patients with COVID-19, a different group would be less prioritized, perhaps at the expense of other equity goals.”
Leonard wrote that the original algorithm did include the majority of residents and fellows within the first 10,000 doses, but Stanford Medicine leadership “did not recognize that essentially none would fall in the first wave [last] week given the impact of age on the allocation.” For this first round of vaccinations, only 5,000 doses were available.
According to a letter written by the Chief Resident Council last week and obtained by The Daily, Stanford Medicine leadership was aware of the error in the algorithm on Tuesday of last week, a few days before vaccine distribution began on Friday.
“When they discovered this mistake, why did they not act on it?” asked internal medicine resident Sharif Vakili in a statement to The Daily. “Did they not recognize it was a mistake? Did lines of communication between administrators and providers break down? Were key stakeholders ignored?”
Sehgal declined to comment on whether leadership was aware of an error in the algorithm itself before releasing first wave lists. “The specific mistake made was that the initial lists were intended for review and they became published and interpreted as final,” he wrote. “We immediately began course correcting on Thursday morning when this was clear.”
Vakili said being a healthcare worker alone should not “entitle us to cut the line for a COVID-19 vaccine.” Given front-line workers need to remain healthy and protected from COVID-19 to manage the pandemic, he said the decision to vaccinate some senior faculty and hospital administrators first was “reckless from a societal standpoint.”
“If you think about it, an outpatient ophthalmologist or especially a hospital administrator has no greater risk of contracting COVID than the cashier at Trader Joe’s,” he wrote. “Unless [healthcare workers are] on the bench to work in any front-line COVID capacity, they should really not be getting these precious very first vaccine doses.”
Stanford Health Care spokesperson Julie Greicius told The Daily that Stanford Health Care administrators David Entwistle, Paul King and Lloyd Minor “have not been vaccinated and do not intend to be vaccinated until all others at Stanford Medicine who want to receive the vaccine are able to do so.”
University spokesperson E.J. Miranda added that the first wave of vaccinations was reserved for Stanford Health Care only and that President Marc Tessier-Lavigne and Provost Persis Drell have not been vaccinated either.
Internal medicine resident Angela Primbas said the lack of transparency regarding the allocation process was also concerning, as residents were not aware of how the vaccines were being distributed or how administrators were making decisions. Residents, attendings, program directors and department chairs were left out of the decision-making process, according to Primbas.
Leonard wrote that the rollout opened up an important dialogue, allowing housestaff and administration to work together to build “longer-term solutions that will be an asset to Stanford Medicine’s Graduate Medical Education program.” She added that the Chief Resident Council will work with leadership to ensure representation through hospital-level committee meetings.
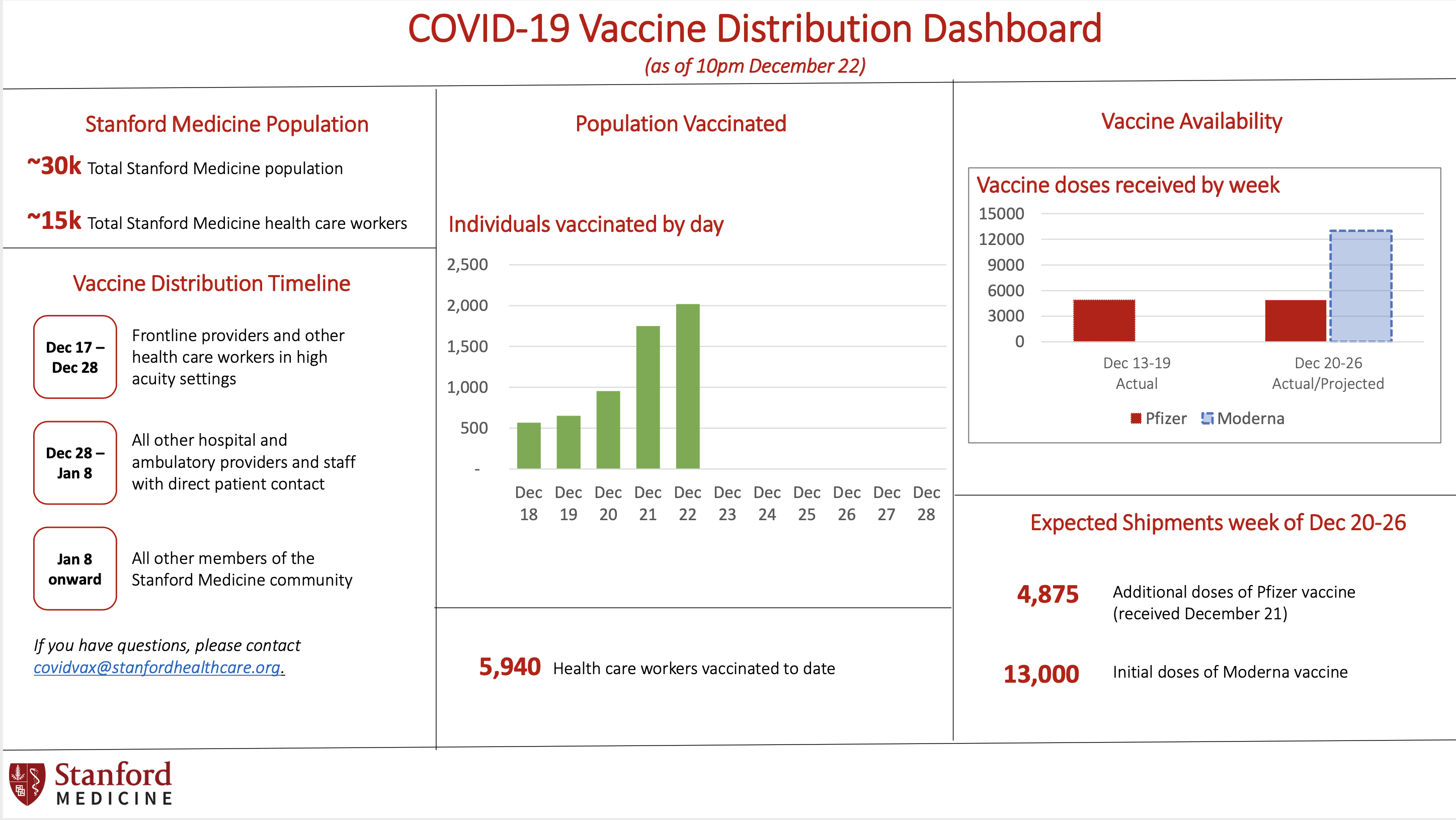
According to a statement released by Stanford Medicine on Sunday, a Vaccine Distribution Dashboard was created to increase transparency surrounding the vaccination process going forward. The dashboard provides a “daily snapshot” of Stanford’s vaccination progress, including a distribution timeline, population vaccinated, vaccine availability and expected shipments.
New allocation method
While the original approach prioritized overall COVID-19 risk factors, the revised approach prioritizes workers in high-risk clinical settings first, according to a letter written jointly by the Chief Resident Council and Stanford Graduate Medical Education leadership to housestaff.
Over the past few days, chief residents from all departments met with hospital administration to ensure “both that vaccines were reallocated and that housestaff had greater representation in hospital leadership and decision-making,” according to the letter.
The new allocation method still takes into account personal risk factors such as age and pre-existing health conditions, but also places more emphasis on healthcare environment risk by identifying three levels of exposure depending on workplace setting –– high-acuity care delivery settings (such as the emergency department, ICU and COVID-19 units), other lower-risk areas of the hospital and ambulatory care and remote settings.
As the new plan is being implemented, those working in COVID-19 wards are now able to walk up and receive accommodations to get vaccinated at any time as long as appointments can be squeezed in, according to residents.
According to Leonard, a consensus among division chiefs, associate chairs and education leadership decided that faculty members who had originally been given vaccine allocations would not get their vaccine until all of the front-line housestaff had received it.
Contact Athena Xue at axue8 ‘at’ stanford.edu and Esha Dhawan at edhawan ‘at’ stanford.edu.
The article has been updated to reflect that Vakili said vaccinating some senior faculty and hospital administrators over front-line workers is “reckless from a societal standpoint” because not all healthcare workers are involved in directly treating COVID-19 patients and managing the pandemic.
The article has been corrected to reflect that the letter outlining the revised allocation approach was written jointly by the Chief Resident Council and Graduate Medical Education leadership. The original article stated the letter was written only by the Chief Resident Council. The Daily regrets this error.